Lipoprotein (a) in Cardiovascular Risk Assessment and Management in Diabetes Mellitus
DOI:
https://doi.org/10.58931/cdet.2023.1315Abstract
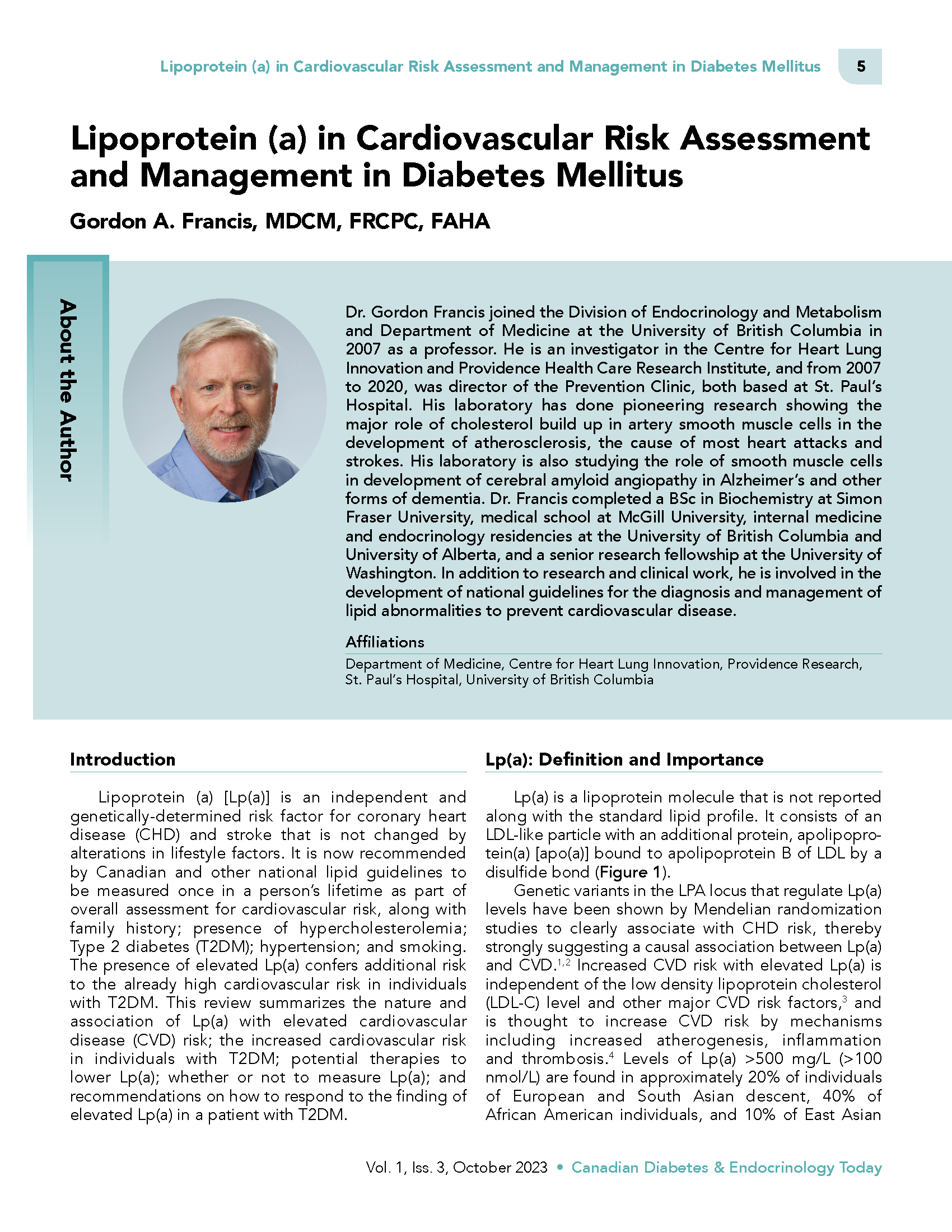
Lipoprotein (a) [Lp(a)] is an independent and genetically-determined risk factor for coronary heart disease (CHD) and stroke that is not changed by alterations in lifestyle factors. It is now recommended by Canadian and other national lipid guidelines to be measured once in a person’s lifetime as part of overall assessment for cardiovascular risk, along with family history; presence of hypercholesterolemia; Type 2 diabetes (T2DM); hypertension; and smoking. The presence of elevated Lp(a) confers additional risk to the already high cardiovascular risk in individuals with T2DM. This review summarizes the nature and association of Lp(a) with elevated cardiovascular disease (CVD) risk; the increased cardiovascular risk in individuals with T2DM; potential therapies to lower Lp(a); whether or not to measure Lp(a); and recommendations on how to respond to the finding of elevated Lp(a) in a patient with T2DM.
References
Clarke R, Peden JF, Hopewell JC, et al. Genetic variants associated with Lp(a) lipoprotein level and coronary disease. N Engl J Med. 2009 Dec 24;361(26):2518–2528. DOI: https://doi.org/10.1056/NEJMoa0902604
Kamstrup PR, Tybjaerg-Hansen A, Steffensen R, et al. Genetically elevated lipoprotein(a) and increased risk of myocardial infarction. JAMA. 2009 Jun 10;301(22):2331–2339. DOI: https://doi.org/10.1001/jama.2009.801
Nordestgaard BG, Chapman MJ, Ray K, et al. Lipoprotein(a) as a cardiovascular risk factor: current status. Eur Heart J. 2010 Dec;31(23):2844–2853. DOI: https://doi.org/10.1093/eurheartj/ehq386
Reyes-Soffer G, Ginsberg HN, Berglund L, et al. Lipoprotein(a): a genetically determined, causal, and prevalent risk factor for atherosclerotic cardiovascular disease: a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol. 2022 Jan;42(1):e48–60. DOI: https://doi.org/10.1161/ATV.0000000000000147
Paré G, Çaku A, McQueen M, et al. Lipoprotein(a) levels and the risk of myocardial infarction among 7 ethnic groups. Circulation. 2019 Mar 19;139(12):1472–1482. DOI: https://doi.org/10.1161/CIRCULATIONAHA.118.034311
Enkhmaa B, Anuurad E, Berglund L. Lipoprotein (a): impact by ethnicity and environmental and medical conditions. J Lipid Res. 2016;57(7):1111–1125. DOI: https://doi.org/10.1194/jlr.R051904
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020 Jan 1;41(1):111–188.
Pearson GJ, Thanassoulis G, Anderson TJ, et al. 2021 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in Adults. Can J Cardiol. 2021 Aug;37(8):1129–1150. DOI: https://doi.org/10.1016/j.cjca.2021.03.016
Booth GL, Kapral MK, Fung K, et al. Relation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: a population-based retrospective cohort study. Lancet. 2006 Jul 1;368(9529):29-36. DOI: https://doi.org/10.1016/S0140-6736(06)68967-8
Low Wang CC, Hess CN, Hiatt WR. Clinical update: cardiovascular disease in diabetes mellitus: atherosclerotic cardiovascular disease and heart failure in type 2 diabetes mellitus - mechanisms, management, and clinical considerations. Circulation. 2016 Jun 14;133(24):2459–2502. DOI: https://doi.org/10.1161/CIRCULATIONAHA.116.022194
Bornfeldt KE. The remnant lipoprotein hypothesis of diabetes-associated cardiovascular disease. Arterioscler Thromb Vasc Biol. 2022 Jul;42(7):819-830. DOI: https://doi.org/10.1161/ATVBAHA.122.317163
Ward NC, Vickneswaran S, Watts GF. Lipoprotein (a) and diabetes mellitus: causes and consequences. Curr Opin Endocrinol Diabetes Obes. 2021 Apr 1;28(2):181-187. DOI: https://doi.org/10.1097/MED.0000000000000597
Zhang HW, Zhao X, Guo YL, et al. Elevated lipoprotein (a) levels are associated with the presence and severity of coronary artery disease in patients with type 2 diabetes mellitus. Nutr Metab Cardiovasc Dis NMCD. 2018 Oct;28(10):980-986. DOI: https://doi.org/10.1016/j.numecd.2018.05.010
Waldeyer C, Makarova N, Zeller T, et al. Lipoprotein(a) and the risk of cardiovascular disease in the European population: results from the BiomarCaRE consortium. Eur Heart J. 2017 Aug 21;38(32):2490-2498. DOI: https://doi.org/10.1093/eurheartj/ehx166
Jin JL, Cao YX, Zhang HW, et al. Lipoprotein(a) and Cardiovascular Outcomes in Patients With Coronary Artery Disease and Prediabetes or Diabetes. Diabetes Care. 2019 Jul;42(7):1312-1318. DOI: https://doi.org/10.2337/dc19-0274
Saeed A, Sun W, Agarwala A, Virani SS, Nambi V, Coresh J, et al. Lipoprotein(a) levels and risk of cardiovascular disease events in individuals with diabetes mellitus or prediabetes: The Atherosclerosis Risk in Communities study. Atherosclerosis. 2019 Mar;282:52-56. DOI: https://doi.org/10.1016/j.atherosclerosis.2018.12.022
Moosaie F, Davatgari RM, Firouzabadi FD, et al. Lipoprotein(a) and apolipoproteins as predictors for diabetic retinopathy and its severity in adults with type 2 diabetes: a case-cohort study. Can J Diabetes. 2020 Jul;44(5):414-421. DOI: https://doi.org/10.1016/j.jcjd.2020.01.007
O’Donoghue ML, Fazio S, Giugliano RP, et al. Lipoprotein(a), PCSK9 inhibition, and cardiovascular risk. Circulation. 2019;19;139(12):1483-1492. DOI: https://doi.org/10.1161/CIRCULATIONAHA.118.037184
Bittner VA, Szarek M, Aylward PE, et al. Effect of alirocumab on lipoprotein(a) and cardiovascular risk after acute coronary syndrome. J Am Coll Cardiol. 2020 Jan 21;75(2):133-1344.
Malick WA, Goonewardena SN, Koenig W, et al. Clinical trial design for lipoprotein(a)-lowering therapies: JACC focus seminar 2/3. J Am Coll Cardiol. 2023 Apr 25;81(16):1633-1645. DOI: https://doi.org/10.1016/j.jacc.2023.02.033
Burgess S, Ference BA, Staley JR, et al. Association of LPA variants with risk of coronary disease and the implications for lipoprotein(a)-lowering therapies: a Mendelian randomization analysis. JAMA Cardiol. 2018 01;3(7):619-627. DOI: https://doi.org/10.1001/jamacardio.2018.1470
Maher VM, Brown BG, Marcovina SM, et al. Effects of lowering elevated LDL cholesterol on the cardiovascular risk of lipoprotein(a). JAMA. 1995 Dec 13;274(22):1771-1774. DOI: https://doi.org/10.1001/jama.274.22.1771
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Canadian Diabetes & Endocrinology Today

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.