GLP-1 Receptor Agonist Use in Pregnancy
DOI:
https://doi.org/10.58931/cdet.2025.3139Abstract
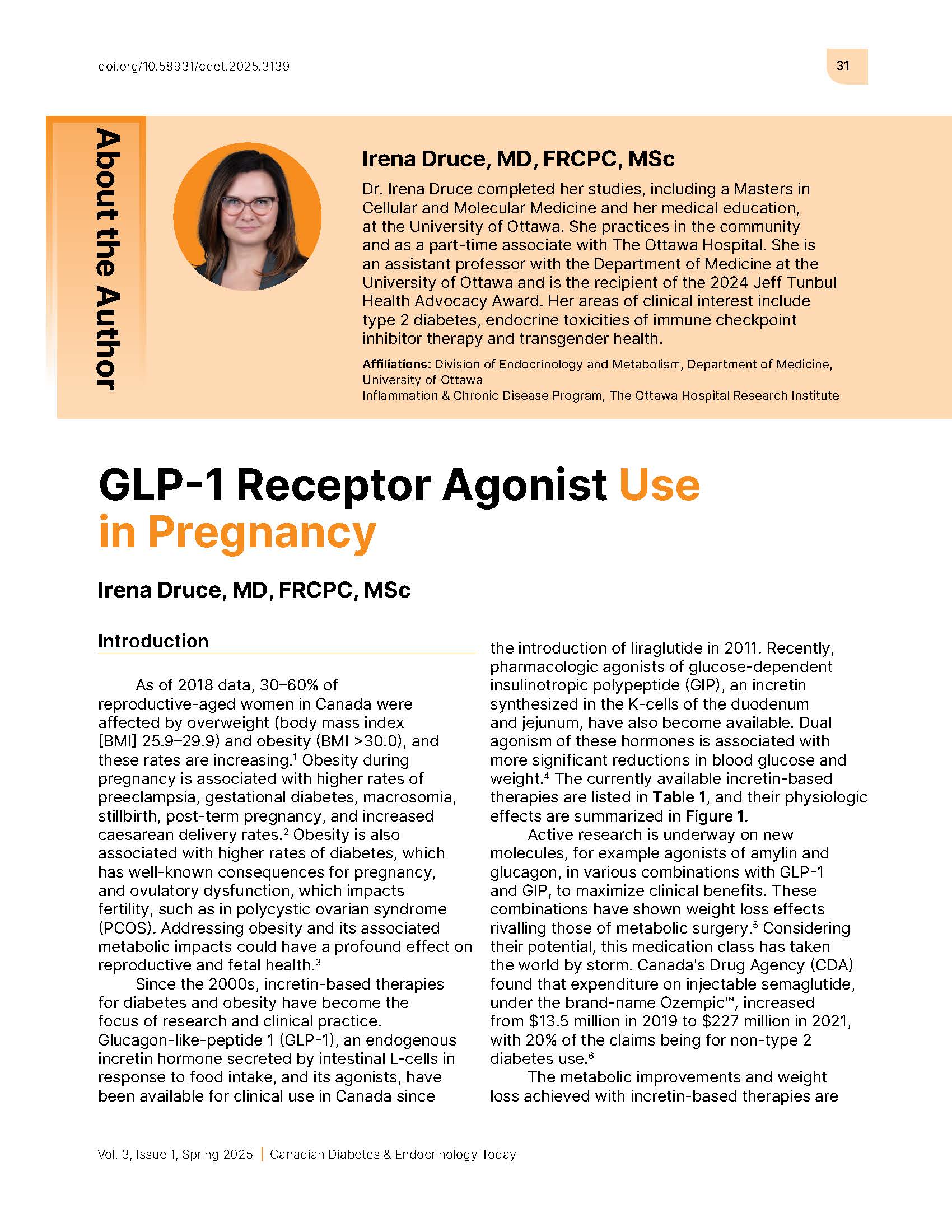
As of 2018 data, 30–60% of reproductive‑aged women in Canada were affected by overweight (body mass index [BMI] 25.9–29.9) and obesity (BMI >30.0), and these rates are increasing. Obesity during pregnancy is associated with higher rates of preeclampsia, gestational diabetes, macrosomia, stillbirth, post‑term pregnancy, and increased caesarean delivery rates. Obesity is also associated with higher rates of diabetes, which has well‑known consequences for pregnancy, and ovulatory dysfunction, which impacts fertility, such as in polycystic ovarian syndrome (PCOS). Addressing obesity and its associated metabolic impacts could have a profound effect on reproductive and fetal health.
Since the 2000s, incretin-based therapies for diabetes and obesity have become the focus of research and clinical practice. Glucagon‑like‑peptide 1 (GLP-1), an endogenous incretin hormone secreted by intestinal L-cells in response to food intake, and its agonists, have been available for clinical use in Canada since the introduction of liraglutide in 2011. Recently, pharmacologic agonists of glucose-dependent insulinotropic polypeptide (GIP), an incretin synthesized in the K-cells of the duodenum and jejunum, have also become available. Dual agonism of these hormones is associated with more significant reductions in blood glucose and weight. The currently available incretin-based therapies are listed in Table 1, and their physiologic effects are summarized in Figure 1.
Active research is underway on new molecules, for example agonists of amylin and glucagon, in various combinations with GLP‑1 and GIP, to maximize clinical benefits. These combinations have shown weight loss effects rivalling those of metabolic surgery. Considering their potential, this medication class has taken the world by storm. Canada's Drug Agency (CDA) found that expenditure on injectable semaglutide, under the brand-name Ozempic™, increased from $13.5 million in 2019 to $227 million in 2021, with 20% of the claims being for non-type 2 diabetes use.
The metabolic improvements and weight loss achieved with incretin-based therapies are associated with improved fertility. While product monographs warn against use in pregnancy and lactation, conception while on these treatments is becoming more common. Considering this increasing reality, this review aims to summarize what is currently known about GLP-1 and GIP agonists and their effects during pregnancy.
References
Statistics Canada. Overweight and Obese Adults, 2018: Statistics Canada; 2018 [updated 2019, cited March 10, 2025]. Available from: https://www150.statcan.gc.ca/n1/pub/82-625-x/2019001/article/00005-eng.htm
Mission JF, Marshall NE, Caughey AB. Pregnancy risks associated with obesity. Obstet Gynecol Clin North Am. 2015;42(2):335-353. doi:10.1016/j.ogc.2015.01.008 DOI: https://doi.org/10.1016/j.ogc.2015.01.008
Drummond RF, Seif KE, Reece EA. Glucagon-like peptide-1 receptor agonist use in pregnancy: a review. Am J Obstet Gynecol. 2025;232(1):17-25. doi:10.1016/j.ajog.2024.08.024 DOI: https://doi.org/10.1016/j.ajog.2024.08.024
Drucker DJ, Holst JJ. The expanding incretin universe: from basic biology to clinical translation. Diabetologia. 2023;66(10):1765-1779. doi:10.1007/s00125-023-05906-7 DOI: https://doi.org/10.1007/s00125-023-05906-7
Jastreboff AM, Kaplan LM, Frias JP, Wu Q, Du Y, Gurbuz S, et al. Triple-hormone-receptor agonist retatrutide for obesity - a phase 2 trial. N Engl J Med. 2023;389(6):514-526. doi:10.1056/NEJMoa2301972 DOI: https://doi.org/10.1056/NEJMoa2301972
Vaanabouathong C, Crotty C, Le K, Eurich D, Dyrda P. CADTH health technology review: current utilization patterns of glucagon-like peptide-1 receptor agonists. Canadian Journal of Health Technologies. 2022;2(9):1-50. DOI: https://doi.org/10.51731/cjht.2022.434
Jensterle M, Janez A, Fliers E, DeVries JH, Vrtacnik-Bokal E, Siegelaar SE. The role of glucagon-like peptide-1 in reproduction: from physiology to therapeutic perspective. Hum Reprod Update. 2019;25(4):504-517. doi:10.1093/humupd/dmz019 DOI: https://doi.org/10.1093/humupd/dmz019
Outeirino-Iglesias V, Romani-Perez M, Gonzalez-Matias LC, Vigo E, Mallo F. GLP-1 increases preovulatory lh source and the number of mature follicles, as well as synchronizing the onset of puberty in female rats. Endocrinology. 2015;156(11):4226-4237. doi:10.1210/en.2014-1978 DOI: https://doi.org/10.1210/en.2014-1978
Artunc-Ulkumen B, Pala HG, Pala EE, Yavasoglu A, Yigitturk G, Erbas O. Exenatide improves ovarian and endometrial injury and preserves ovarian reserve in streptozocin induced diabetic rats. Gynecol Endocrinol. 2015;31(3):196-201. doi:10.3109/09513590.2014.975686 DOI: https://doi.org/10.3109/09513590.2014.975686
Szczesnowicz A, Szeliga A, Niwczyk O, Bala G, Meczekalski B. Do GLP-1 analogs have a place in the treatment of PCOS? New insights and promising therapies. J Clin Med. 2023;12(18):5915. doi:10.3390/jcm12185915 DOI: https://doi.org/10.3390/jcm12185915
Siamashvili M, Davis SN. Update on the effects of GLP-1 receptor agonists for the treatment of polycystic ovary syndrome. Expert Rev Clin Pharmacol. 2021;14(9):1081-1089. doi:10.1080/17512433.2021.1933433 DOI: https://doi.org/10.1080/17512433.2021.1933433
Pedersen SD, Manjoo P, Wharton S. Canadian Adult Obesity Clinical Practice Guidelines: Pharmacotherapy for Obesity Management. Available from: https://obesitycanada.ca/guidelines/pharmacotherapy.
Qiao L, Lu C, Zang T, Dzyuba B, Shao J. Maternal GLP-1 receptor activation inhibits fetal growth. Am J Physiol Endocrinol Metab. 2024;326(3):E268-E276. doi:10.1152/ajpendo.00361.2023 DOI: https://doi.org/10.1152/ajpendo.00361.2023
Younes ST, Maeda KJ, Sasser J, Ryan MJ. The glucagon-like peptide 1 receptor agonist liraglutide attenuates placental ischemia-induced hypertension. Am J Physiol Heart Circ Physiol. 2020;318(1):H72-H77. doi:10.1152/ajpheart.00486.2019 DOI: https://doi.org/10.1152/ajpheart.00486.2019
Graham DL, Madkour HS, Noble BL, Schatschneider C, Stanwood GD. Long-term functional alterations following prenatal GLP-1R activation. Neurotoxicol Teratol. 2021;87:106984. doi:10.1016/j.ntt.2021.106984 DOI: https://doi.org/10.1016/j.ntt.2021.106984
Price SAL, Nankervis A. Considering the use of GLP-1 receptor agonists in women with obesity prior to pregnancy: a narrative review. Arch Gynecol Obstet. 2025. doi:10.1007/s00404-024-07849-9 DOI: https://doi.org/10.1007/s00404-024-07849-9
Ivanisevic M, Herman M, Horvaticek M, Vucic Lovrencic M, Delmis J. Pregnancy outcome and liraglutide levels in serum and umbilical vein blood of a woman with type 2 diabetes. A case report. Gynaecol Perinatol. 2018;27(3-4):70-72.
Cesta CE, Rotem R, Bateman BT, Chodick G, Cohen JM, Furu K, et al. Safety of GLP-1 receptor agonists and other second-line antidiabetics in early pregnancy. JAMA Intern Med. 2024;184(2):144-152. doi:10.1001/jamainternmed.2023.6663 DOI: https://doi.org/10.1001/jamainternmed.2023.6663
Dao K, Shechtman S, Weber-Schoendorfer C, Diav-Citrin O, Murad RH, Berlin M, et al. Use of GLP1 receptor agonists in early pregnancy and reproductive safety: a multicentre, observational, prospective cohort study based on the databases of six Teratology Information Services. BMJ Open. 2024;14(4):e083550. doi:10.1136/bmjopen-2023-083550 DOI: https://doi.org/10.1136/bmjopen-2023-083550
Dumolt JH, Rosario FJ, Kramer AC, Horwitz S, Powell TL, Jansson T. Maternal glucagon-like peptide-1 is positively associated with fetal growth in pregnancies complicated with obesity. Clin Sci (Lond). 2023;137(8):663-678. doi:10.1042/CS20220890 DOI: https://doi.org/10.1042/CS20220890
Kubota S, Yabe D. Elevation of Fasting GLP-1 Levels in Child and Adolescent Obesity: Friend or Foe? J Clin Endocrinol Metab. 2021;106(9):e3778-e3780. doi:10.1210/clinem/dgab301 DOI: https://doi.org/10.1210/clinem/dgab301
Chapter 1 Contraception in Canada. J Obstet Gynaecol Can. 2015;37(10 Suppl):S5-S12. doi:10.1016/S1701-2163(16)39370-7 DOI: https://doi.org/10.1016/S1701-2163(16)39370-7
Skelley JW, Swearengin K, York AL, Glover LH. The impact of tirzepatide and glucagon-like peptide 1 receptor agonists on oral hormonal contraception. J Am Pharm Assoc (2003). 2024;64(1):204-211 e204. doi:10.1016/j.japh.2023.10.037 DOI: https://doi.org/10.1016/j.japh.2023.10.037
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Canadian Diabetes & Endocrinology Today

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.